Weight Loss for Kids and Teens
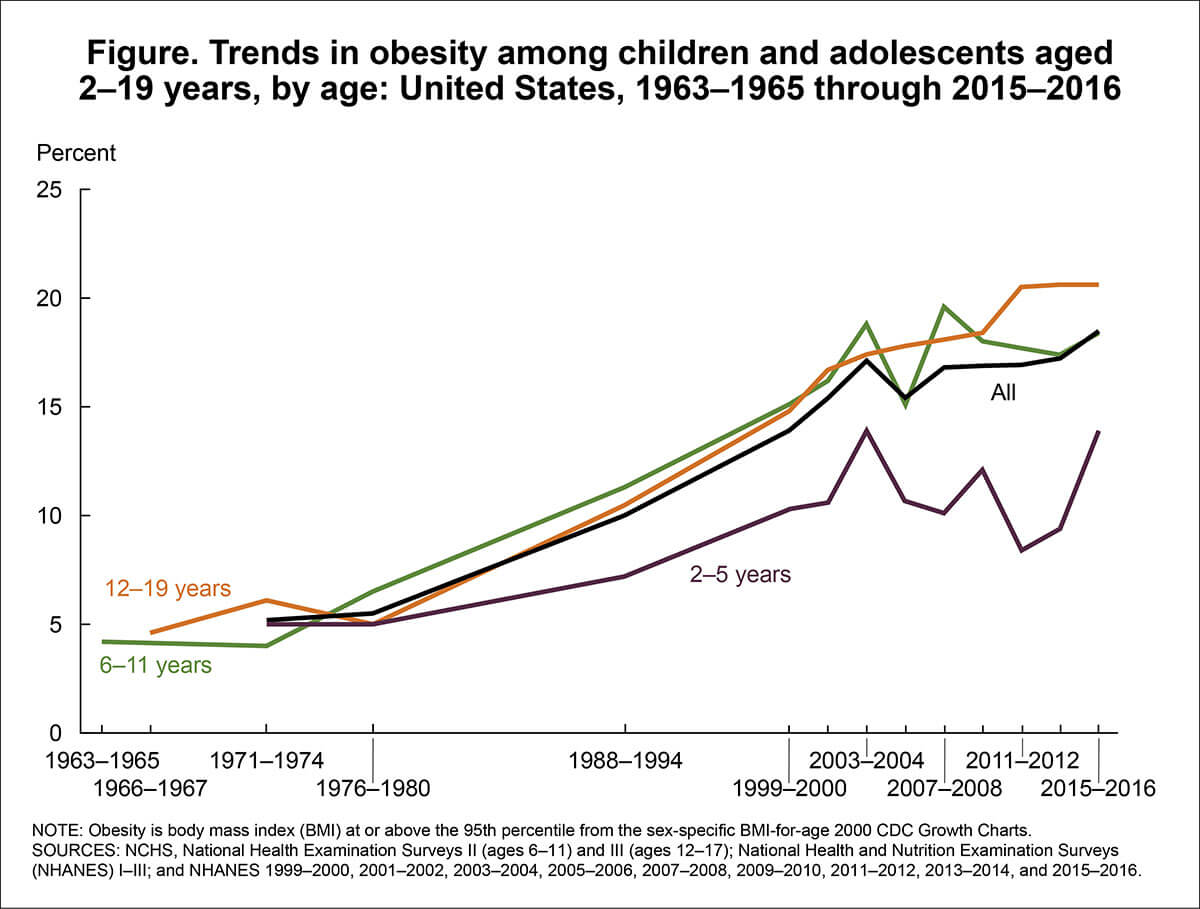
Teen obesity is continuing to rise in parallel to the rise in adult and childhood obesity. Obesity in children and teens is increasing much faster than in adults. In the 1970’s only 6% of children were overweight, while in 2017 more than 30% were found to be overweight or obese. Weight loss for kids and teens, and preventing them from becoming overweight, becomes more important every day.
Why are so many teens becoming overweight and obese?
Despite a very high metabolism and the fact that teens are growing, its easy to consume hundreds of excess calories. The body will store these extra calories and fat builds up in the body. Being overweight and obese means a high risk for developing other health problems. Obesity is becoming a serious issue in the United States today, and about one-third of teenagers are overweight or obese. Binge eating, purging, and even anorexia and bulimia are becoming common in teens. Eating in secret is one of the ways teens are able to gain weight without parental knowledge.
Weight Loss for Kids & Teens Diet Plan
Dr. Lipman has helped many teens and older children that are overweight as part of his family obesity plan. When treating one or more of the overweight parents, teens and older children in the family are encouraged to participate in dietary changes.
Dr. Lipman is not a pediatrician. He sees children from ages 10-16 only at the same time as part of a family with one or more obese parents. Severely obese children (BMI > 30) need to see their own doctor or pediatric weight loss specialist.
The Weight Loss for Kids & Teens Diet Plan is a modified version of the Miami Diet Plan. After a medical evaluation, we talk to your child about their eating habits. From there we determine their diet secrets and trigger foods. With all of that information, Dr. Lipman designs a simple, easy-to-follow diet plan with foods kids and their families can all enjoy. This plan has no complicated points systems, no counting carbs or fats or calories, no exotic food, and no expensive branded meals.
Recognizing Overeating in Teens and Kids is the First Step to Helping Them Lose Weight
The first step in helping overweight children is to learn how to recognize the problem. Most parents think their overweight children are “just about normal.” It is very normal for parents to erect barriers to prevent them from enforcing eating rules in their children. Parents are used to feeding and nourishing their young and have great difficulties recognizing childhood obesity at home. Doing something about it is even more difficult.

Nothing can be done to help children and teens with their dysfunctional eating problems until the parents are willing to recognize and accept the fact that their child or teen is overeating, overweight or obese. No matter what the type of eating dysfunction, it needs to trigger a reaction in the parents to make changes in the whole family’s eating and drinking.
Sixty three percent of parents (higher if the parents are both overweight) fail to recognize their child is overweight or obese despite the child’s obvious physical appearance. Often they perceive their child’s excess weight to be a temporary problem – “baby fat” or a “stage” which they are sure they will “outgrow”. Many feel that weight loss for kids is not necessary or just cosmetic.
Only 4% of parents in the US are willing to admit that their child is even a little overweight, when, in fact, 33 % of all children in this country are overweight or obese. Secretive eating, binge eating, sedentary lifestyle, and unhealthy or fast food meals are often the source of excess calories.
A Growing Problem in the United States
Since 1963, childhood obesity rates have quadrupled. Below are just some of the research studies and statistics collected by the CDC relating to the obesity epidemic in the United States, as well as childhood obesity. Weight loss for children and teens is more important now than it has ever been. Recognizing that your child is overweight and taking action is the best thing you can do to help them live a longer, healthier life.
- Trends in Obesity/overweight from Health, United States
- Prevalence of Overweight, Obesity, and Severe Obesity Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2015–2016
- Attempts to Lose Weight Among Adults in the United States, 2013–2016
- Prevalence of High Weight-for-recumbent Length Among Infants and Toddlers From Birth to 24 Months of Age: United States, 1971–1974 Through 2013–2014
- Prevalence of Overweight and Obesity Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2013–2014
- Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults Aged 20 and Over: United States, 1960–1962 Through 2013–2014
- Prevalence of Obesity Among Children and Adolescents in the United States and Canada.
- Perception of Weight Status in U.S. Children and Adolescents Aged 8–15 Years, 2005–2012
- Prevalence of Obesity Among Older Adults in the United States, 2007–2010
- Prevalence of Low Weight-for-recumbent Length, Recumbent Length-for-age, and Weight-for-age Among Infants and Toddlers From Birth to 24 Months of Age: United States, 1999–2000 Through 2013–2014
- Prevalence of Underweight Among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 Through 2013–2014
- Prevalence of Underweight Among Adults Aged 20 and Over: United States, 1960–1962 Through 2013–2014
- Current Asthma Prevalence by Weight Status Among Adults: United States, 2001–2014
- Characteristics of Physician Office Visits for Obesity by Adults Aged 20 and Over, United States, 2012
Using Teen or Child’s Waist Line to Recognize Overeating, Overweight, and Obesity
Waist circumference in teens and older children, more so than in adults, is a better indicator of overeating and possibly becoming overweight or obese.
The metabolic disorders accompanying weight gain and the associated risks are more directly related to waist circumference than weight or BMI. Recent reports on the distribution of waist circumferences for children between 2 and 18 years old revealed waist circumferences values of 26 inches for 6 year old boys and girls and 33 inches for 12 year old boys and 32 inches for 12 year old girls were the cutoff between normal and overweight children (the 90th percentile). Note that the normal child increases his/her waist line about 1 inch a year as he/she gains weight.
While data on waist circumferences is not as extensive in children as in adults, there are enough studies to make some generalizations. Pediatricians treating obesity usually make little distinction between overweight and obese. Instead, they prefer to place the child into a category labeled “overweight” which includes both groups of children, since the treatment is the same.

On the left of the graph (Y-Axis) is waist circumference and on the bottom (X-Axis) is age. Below the purple line is normal, overweight is between the purple and green lines, and above the green line indicates obesity.
Using Body Mass Index (BMI) for Older Children and Teens
Body mass index (BMI) is a good measurement for determining if a person is overweight. Try the BMI calculator on this page to check you or your child’s BMI. BMI considers a person’s height and weight to estimate body fat. Once your BMI is calculated you can compare it to a BMI chart. The BMI chart for kids and teens is a bit different than the chart for adults. If a child’s BMI falls above the 85th percentile but less than the 95th he or she is considered overweight. If it is above the 95th percentile, the child is considered obese.

Overweight Teens Become Overweight Adults
According to the United States Department Health and Human Services, 7 out of 10 overweight adolescents will become overweight adults. If one parent is overweight it rises to 8 out of 10. Ninety percent of parents were unable to estimate their child’s weight accurately and most do not appreciate the health risks of childhood obesity. Some parents think being underweight is more dangerous than being overweight (a very old fashioned view). Some parents think their overweight child’s problem are no more serious than a “bad cold”. This lack of acknowledgement makes the importance of weight loss for kids even more difficult to communicate.
The latest US government statistics show that among the 335 million Americans, 64% of women and 74% of men are either overweight or obese. About 34% of children and teens fall into these groups. That would mean that among the 115 million American households, about 3/4 of them would have one or more overweight adults. There are about 25-30 million American households with overweight children or teens as well as one or more overweight parents. This is the group of overeating Americans that are so hard to reach.
Weight Loss for Kids & Teens: Heredity and Example
Body weight is second after height as one of the more important heritable factors. With one parent overweight the odds a child being overweight is 50%, and with two parents overweight it rises to 90% or more.
All of this data provides evidence that the children will follow the same path as their parents. The parental eating patterns are reproduced in the child. Starting to change this means that the parents have to recognize that they need to lose weight and that their children or teens need to at least slow down their weight gain. Since the average child or teen gains between 6-10 lbs. a year normally, often it’s simply a matter of slowing down the weight gain. That way, in a year or two they will arrive at a normal or close to normal weight.
Part of this blindness is the result of fears parents have about using pejorative terms about their children. This is even more difficult if they too were overweight as a child. Even physicians are concerned with angering or upsetting the parents in these situations.
Doctors Fail to Recognize and Help Overweight Teens
Doctors are even worse than parents. Researchers at the Mayo Clinic reviewed the charts of 2500 overweight patients who had just seen their doctor. Only 20% of the obese people were recognized as obese. Those that had their weight problem recognized were twice as likely to lose weight.
According to a 2005 study in the journal Pediatrics, doctors diagnosed obesity less than 1% of the time among 2-to-18-year-olds – a figure far below the one-third of young Americans struggling with weight. Another study in 2005 indicated that only 12% of pediatricians were effective in helping overweight children. It is a sensitive area on all sides.
Poor Communication With Family Doctor
Overall, just 9% of adults interviewed by Consumer Reports said that a physician had suggested that their child or teen lose weight. Among respondents with kids more than 20% overweight, 51% reported that their physician had suggested their child shed some pounds. That leaves almost half of all parents of severely overweight kids not engaging in a dialogue with their family doctor about their child’s weight problem.
Weight Loss for Kids and Teens: What You Can Do
It all starts with the parents. If they suspect their child is overeating or overweight, then they need to measure the child or teen’s waist line. If they are borderline or overweight, then they need to approach their family doctor with the facts. Nothing can be done until the overeating and poor food choices are recognized and nothing can be done unless there is a plan.
A recent large investigation uncovered that being overweight is a very difficult subject for parents to discuss with their teens. One in 20 parents of adolescents said that they are struggling with their teens’ use of drugs, alcohol, and smoking. However, more than 25% of parents are hesitant to talk to their teens about their overeating and weight gain. The study suggested that parents of kids ages 8 to 17 avoid the subject of weight completely. One in five parents admit they have never brought up the subject of maintaining a healthy weight despite knowing that being overweight poses an immediate health risk to their kids. Ninety percent of healthcare professionals said that maintaining a healthy weight is the most important health topic that parents should discuss with their children. One in 5 parents said that their doctor should be the one to discuss the dangers of being overweight.
Susan Bartell, Psy.D., an obesity expert, writes:
“Weight has become such an emotionally charged and pervasive subject, especially in a culture that is highly image-driven. Broaching this subject can be extremely intimidating for parents, especially given that parents themselves may be struggling with their weight.”
Parents Can Start Listening to Their Kids and Teens
Given these facts, the first step is for parents to start listening to their kids. No system works better for weight loss for kids and teens than recognizing themselves that they weigh too much and want to do something about it.
In Their Own Words: How Real Kids and Teens Express Their Unhappiness About Being Overweight
It’s important for parents to understand that kids, just like adults, often don’t like to talk about their weight. Additionally, with social pressures to look a certain way or to love your body just the way it is, the messages of good health and risks of obesity often get lost. It is never “shaming” your children to want them to reach a healthy weight and also helping them achieve it. It’s all in how you talk to them about it and the example you set.
If you hear any of these comments, don’t ignore it. It might have taken months for them to get the courage to say it. Ask them if they would like to see a doctor to find out what weight is “normal” for their age and height. You can also ask if they would like help starting a fun exercise program. Invite them to go with you to the supermarket to help you find new foods to try that they might enjoy.
Problems Children Share with Adults
- “My clothes are too tight and I need new clothes every month.”
- “I can’t find anything that fits me.”
- “I never wear a bathing suit and avoid pool and beach parties.”
- “I hate to look in the mirror or have pictures taken of myself.”
- “I like loose clothes and wear oversize shirts to cover my belly.”
- “Every one of my friends is skinny and can wear the coolest clothes.”
- “I am so ashamed to talk about my weight.”
- “Other kids make fun of my weight/size.”
- “I suddenly lose my friends and have trouble finding new ones.”
- “I don’t get invited to birthday parties or to friend’s houses.”
- “I feel uncomfortable/awkward with members of the opposite sex.”
- “I can’t keep up in sports; nobody wants me on their teams at school.”
- “I get short of breath and feel tired all day, I fall asleep in class.”
- “I have stretch marks and saggy skin.”
- “I can’t fit into the desks at school.”
More Worries That Overweight Teens Share With Their Friends
- “I really want to lose weight, but I’m too ashamed to tell my family. I know they will talk about me behind my back and make fun of me.”
- “People I thought were my friends are making fun of my weight on Instagram and Facebook.”
- “I hate my fat body.”
- “Sometimes I feel like I can’t control myself once I start eating.”
- “How do I stop craving (favorite junk food)?”
- “Why do I still gain weight when I’m eating healthy?”
- “What if you’re exercising and eating healthy but you’re still gaining weight?”
- ”I eat when I am bored.”
- “I’m afraid my other friends or family won’t support me trying to lose weight.”
- “How do you know when to stop eating? Clean plate? Empty bag?”
- “I have stretch marks that make me look like I was pregnant.”
- “I am going to see my doctor, but I’m afraid that when I get on the scale I will hear long lectures from my mom. I know I am fat and it’s unhealthy”
- “Last year no one came to my birthday party. Maybe because I am 200 lbs. and am only 13.”
- “My mom saw my big belly and thought I was pregnant”
- “I am so embarrassed. I broke a chair at school because I weigh so much.”
- “I am 16 and weigh 220 lbs. I know I need to lose weight, but I don’t know how to even start. What should I do?”
- “Everyone thinks I’m lazy and stupid because I weigh so much. That’s not true. How do I tell my teachers I’m just like everyone else?”
- “You are the only one I can talk to about my terrible sugar cravings.”
Dr. Lipman’s 12 Warning Signs Your Child Has a Problem With Overeating
- His/her doctor tells you so.
- Your child complains about being teased about her/his size.
- Your child’s clothes seem to get too small too fast.
- Shopping for clothes with your child is a nightmare.
- Your child refuses to be seen in a bathing suit.
- Your child’s friendships are suddenly changing.
- Your child withdraws from activities he/she previously enjoyed.
- You find yourself referring to him/her as “big-boned” or “large.”
- You notice your child huffing and puffing after a simple task such as climbing a flight of stairs.
- You keep telling your child or teen to stop eating.
- Your child insists on ordering from a restaurant adult menu
- Your child tells you she or he is over-weight.
Remember, if you hear your child saying things like this, don’t ignore it. They are asking for your help.